
Analysis of modified double-bundle anterior cruciate ligament reconstruction with
implantless fixation on tibial side
Skand Sinha, Ananta K. Naik, Appan Kumar, Tista Jacob, Santanu Kar
PII: S1008-1275(20)30114-0
DOI: https://doi.org/10.1016/j.cjtee.2020.04.007
Reference: CJTEE 461
To appear in: Chinese Journal of Traumatology
Received Date: 21 November 2019
Revised Date: 8 December 2019
Accepted Date: 10 December 2019
Please cite this article as: Sinha S, Naik AK, Kumar A, Jacob T, Kar S, Analysis of modified doublebundle anterior cruciate ligament reconstruction with implantless fixation on tibial side, Chinese Journal
of Traumatology, https://doi.org/10.1016/j.cjtee.2020.04.007
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition
of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of
record. This version will undergo additional copyediting, typesetting and review before it is published
in its final form, but we are providing this version to give early visibility of the article. Please note that,
during the production process, errors may be discovered which could affect the content, and all legal
disclaimers that apply to the journal pertain.
© 2020 Production and hosting by Elsevier B.V. on behalf of Chinese Medical Association.
Analysis of modified double-bundle anterior cruciate ligament reconstruction with implantless fixation on
8 tibial side
Skand Sinhaa, *, Ananta K Naikb
, Appan Kumarb
, Tista Jacobb
, Santanu Karb
9
10
a
11 Sports Injury Centre, Safdarjung & VMMC, New Delhi 110029, India
b
12 Department of Orthopaedics, PGIMER & Dr RML Hospital, New Delhi 110001, India
*Corresponding author. Email address: skandsinha@gmail.com
Abstract
Purpose: To avoid potential problems of double-bundle anterior cruciate ligament reconstruction (ACLR),
18 various modifications have been reported. This study analyzed a novel technique of modified double-bundle
19 (MDB) ACLR without implant on tibial side in comparison to single-bundle (SB) ACLR.
Methods: Eighty cases of isolated anterior cruciate ligament tear (40 each in SB or MDB group) were
21 included. SB ACLR was performed by outside in technique with quadrupled hamstring graft fixed with
22 interference screws. In MDB group, ACLR harvested tendons were looped over each other at the center and
23 free ends whipstitched. Femoral tunnel was created by outside in technique. Anteromedial tibial tunnel was
24 created with tibial guide at 55 degrees. The anatomic posterolateral aiming guide (Smith-Nephew) was used
25 to create posterolateral tunnel. With the help of shuttle sutures, the free end of Gracillis was passed through
26 posterolateral tunnel to femoral tunnel followed by semitendinosus graft through anteromedial tunnel to
27 femoral tunnel. On tibial side the graft was looped over bone-bridge between external apertures of
28 anteromedial and posterolateral tunnel. Graft was fixed with interference screw on femoral side in 10
29 degrees knee flexion. International Knee Documentation Committee (IKDC), Tegner score, Pivot shift and
knee laxity test (KLT, Karl-Storz) were recorded pre- and post-surgery. At one year MRI was done.
Statistical analysis was done by SPSS software.
Results: Mean preoperative KLT reading of (10.00 ± 1.17) mm in MDB group improved to (4.10 ± 0.56)
33 mm and in SB group it improved from (10.00±0.91) mm to (4.80 ± 0.46) mm. The mean preoperative IKDC
34 score in MDB group improved from (49.49 ± 8.00) to (92.5 ± 1.5) at one year and that in SB group
35 improved from (52.5 ± 6.9) to (88.4 ± 2.6). At one-year 92.5% cases in MDB group achieved their preinjury
36 Tegner activity level as compared to 60% in SB group. The improvement in IKDC, KLT and Tegner scale
37 of MDB group was superior to SB group. MRI confirmed graft integrity at one year and clinically at 2 years.
Conclusion: MDB ACLR has shown better outcome than SB ACLR. It is a simple technique that does not
39 require fixation on tibial side and resultant graft is close to native ACL
Keywords: Anterior cruciate ligament reconstruction, Fracture fixation, Tibia
Introduction : 43 Arthroscopic anterior cruciate ligament reconstruction (ACLR) is a major area of research worldwide. Double44 bundle (DB) ACLR has been shown to be superior to conventional single-bundle (SB) technique, as both
bundles act in synergistic way in response to anterior tibial and combined rotatory loads.1 45 Anteromedial bundle
46 is taut through out range of motion of the knee as anteromedial femoral foot print is the most isometric point on
47 femoral side but posterolateral bundle is taut in extension and relaxed in flexion.
48 Though superior to SB ACLR, DB ACLR has potential risks of tunnel confluence, slippage of small diameter
49 graft and overstuffing of notch especially in small knees. There could be osteonecrosis of the lateral femoral
condyle and difficult revision surgery.2
50
51 To get advantage of DB construct that is having different tension pattern in fibers at different arc of motion of
52 the knee but obviates potential difficulties of the double bundle technique, various modifications have been
reported. These modifications are single tibial double femoral tunnel construct3
53 , single tunnel double bundle
construct,4
single femoral double tibial tunnels with hamstring graft,5,6 54 single femoral double tibial tunnels with
quadriceps graft7, 8 and single femoral single branched tibial tunnel with hamstring graft.9
55 Authors with all of
these modifications have documented satisfactory results. Papachristou et al.5
56 reported ACL reconstruction with 13 61 in cadaveric study documented significantly better rotational
62 stability in reverse “Y” plasty ACLR at varying degrees of knee flexion in comparison to SB ACLR. There is a
63 paucity of literature comparing this graft construct (single femoral double tibial tunnels) with SB ACLR in
64 clinical setting.
65 This study analyzed modified DB ACLR (single femoral double tibial tunnels) using autogenous free
hamstring graft, without implant on tibial side in comparison to SB ACLR in clinical setting. This is the first
67 study to compare results of modified DB ACLR with SB ACLR in clinical setting to the best of our
68 knowledge. We aim to clarify whether the clinical outcome of modified DB ACLR is better than single SB
69 ACLR.
Methods
72 This prospective study was conducted after institutional approval. There were 80 subjects (40 cases in each
73 group) of isolated anterior cruciate ligament tear with the age ranging from18 to 50 years. ACL tear with
74 associated other ligament injuries, cartilage lesions and intra-articular fractures and meniscal tear were
75 excluded. All cases were enrolled consecutively between September 2016 and September 2017. The same
76 surgical team operated all cases. Surgeons not involved in the surgery did the scoring.
Technique of modified DB ACLR
78 After surgical preparation, semitendinosus and Gracillis were harvested through a longitudinal split in
79 aponeurosis of Sartorius along the long axis of hamstrings.
80 Muscle tissue was cleared from each tendon in a standard way. The tendons were doubled over each other at
81 the center of length of each tendon. Free tails of each tendon were whipstitched (Fig. 1). The diameter of
82 graft (doubled semitendinosus, doubled Gracills & quadrupled graft) was measured. The length of prepared
83 graft was also measured. If the composite graft length is short, a fiber tape loop can be used to increase the
length of graft by passing through the individual loop of graft.
85 Standard anteromedial and anterolateral portals are set up. Arthroscopic clearing of joint was done but
86 remnant footprints were preserved as much as possible. With the knee placed in 90 degrees of flexion,
87 outside in ACL femoral guide was placed over femoral footprint of ACL. Starting at the flare of the femoral
88 metaphysis, the guide pin was drilled from outside to inside and its intra-articular exit at anatomical femoral
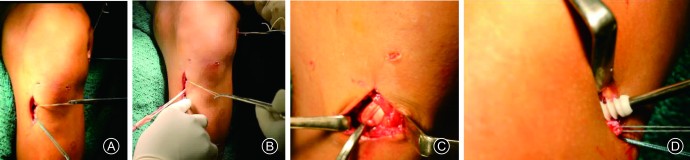
89 footprint is confirmed. The femoral guide was removed. A 2-cm incision was made at the entry point of pin
90 over lateral aspect of the thigh and sequential reaming was done over the pin with the appropriate size
91 reamer to match the diameter of quadrupled hamstrings. A sleeve was placed in femoral tunnel and stationed
92 there.
93 Standard tibial guide set at 55 degrees was placed over anteromedial tibial footprint and the intra-articular
94 exit of guide wire at anteromedial footprint was confirmed. Tibial anteromedial tunnel was reamed
95 according to the size of doubled semitendinosus graft. The anteromedial bullet of the size of anteromedial
96 tibial tunnel was attached to anatomic posterolateral aiming tibial guide (Smith-Nephew).The anteromedial
97 bullet is now inserted in anteromedial tunnel. A guide wire was passed through posterolateral sleeve of the
98 anatomic posterolateral aiming tibial guide. The intra-articular position of guide wire through posterolateral
99 tibial footprint was confirmed (Fig. 2). The posterolateral tunnel was drilled according to the size of doubled
Gracillis.
101 A non-absorbable suture loop was passed through the femoral tunnel from outside and retrieved into the
102 joint through anteromedial portal. A suture retriever was passed through posterolateral tibial tunnel and
103 suture loop in the joint was retrieved through exterior aperture of posterolateral tibial tunnel. Similar process
104 was repeated with another suture loop that was passed from external aperture of femoral tunnel through
105 anteromedial tibial tunnel to exterior (Fig. 3A).
106 The suture tail of sutured free end of Gracillis was passed through suture loop shuttle coming out of
107 posterolateral tibial tunnel. The suture tail of sutured semitendinosus was passed through suture loop shuttle
108 coming out of anteromedial tibial tunnel. Both shuttle sutures were pulled one by one out of femoral tunnel
109 to exterior to deliver free tails of sutured semitendinosus and Gracillis. The posterolateral bundle was seated
110 first by pulling its sutured end (Fig. 3B) followed by anteromedial bundle in similar fashion. Because 13 forms a bridge between external tibial apertures of anteromedial and posterolateral tibial tunnels (Fig. 3C).
114 Because the doubled semitendinosus is longer than doubled Gracillis, the chances of graft being short on
115 anteromedial side are less.
116 After graft was firmly seated, cycling was performed. The graft was fixed on femoral side by bioresorbable
117 interference screw by outside in technique at 10º of flexion of the knee (Fig. 3D). Intra-articular graft is
118 checked (Fig. 4).
119 After thorough lavage of joint, the wound was closed and dressing was done.
Technique of DB ACLR
The free autogenous hamstring harvest was similar to MDB but prepared in a 4-tail graft and dimensions
were measured. Femoral tunnel was prepared as in MDB group. The tibial guide set at 50o 122 was placed at the
123 center of tibial foot print and guide wire passed. The tunnel was created as per size of graft. Graft passage
124 and femoral side fixation was done similar to MDB group. After femoral side fixation, cycling was done,
and then tibial side fixation was done with bioresorbable interference screw in 25o 125 flexion of the knee.
126 Knee was immobilized in full extension with a knee brace. Routine analgesics and antibiotics were given
127 during postoperative period.
Standard accelerated rehab protocol was instituted. Full weight bearing was encouraged as soon as possible.
129 Routine follow-up was done at 2 weeks, 6 weeks, 3 months and 12 months. After 12 months, follow-up was
continued to detect any subjective or objective instability of the knee.
Measurement of outcome
133 year follow-up. Objective measurement of anterior tibial translation was performed preoperatively and at
134 one-year follow-up by a knee laxity tester (KLT, Karl-Storz model No.28729). Manual Pivot shift test was
135 also performed. At one-year follow-up, MRI was done to check for graft integrity. Statistical analysis was
136 done with SPSS software version 13 (SPSS Inc USA). At two-years follow-up, subjective or objective
137 instability if any was noted.
Results
140 There were 40 cases in each group, the age ranging from 18 to 50 years with a mean of (26.82 ± 7.53) years in
141 MDB group and (27.65 ± 7.89) years in SB group. All were males in MDB group and 11 cases (27.5%) were
142 females in SB group. Mean follow-up was (28.97 ± 3.37) months for MDB group and (29.22 ± 3.60) months for
SB group
The mode of injury was variable. Nineteen cases in MDB group and 17 cases in SB group had fall from bike; 15
145 cases in MDB group and 7 cases in SB group had injury during sports; 4 cases in MDB group and 8 cases in SB
146 group had fall on ground; 2 cases in each group had fall from height and 6 cases in SB group had fall at stairs. 13 cases in SB group had mid substance tear, 35 cases in MDB
148 group and 25 cases in SB group had tear at the femoral attachment of ACL and 2 cases in SB group had tear at
149 tibial insertion. The mean time interval between injury and surgery was (16.08 ± 9.29) months in MDB group
150 and (11.70 ± 16.33) months in SB group.
In MDB group the mean composite length of doubled semitendinosus and Gracillis was (253.71+14.01) mm.
152 Twenty-three cases (57.5%) had graft length between 251-275 mm and 14 cases (35%) had graft length between
153 225-250 mm. It was more than 275 mm in one case (2.5%) and less than 225 mm in two cases (5%). The
154 diameter of doubled ST (for AM bundle) was 6 mm in 24 cases (60%), 7 mm in 15 cases (37.5%) and 8 mm in
155 one case (2.5%). The diameter of doubled Gracillis (for PL bundle) was 5 mm in 24 cases (60%) and 6 mm in
156 14 cases (35%).
All cases in both groups could achieve stable knee. The mean preoperative KLT reading in MDB group was
158 (10.00±1.17) mm that improved to (4.1 ± 0.56) mm at follow-up. The mean preoperative KLT reading in SB
159 group was (10.00 ± 0.91) mm that improved to (4.80 ± 0.46) mm. The magnitude of improvement in KLT
160 reading was better in MDB group than SB group with statistical significance. Pivot shift test was negative in all
161 cases of both groups till final follow-up.
162 The mean preoperative IKDC score in MDB group was (49.49 ± 8.00) and it improved to (92.5 ± 1.5) at one
163 year. The mean preoperative IKDC score in SB group was (52.5 ± 6.9) and it improved to (88.4 ± 2.6) at one
164 year. 13 cases, level 2 in 20 cases and level 1 in 7
169 cases. Postoperative Tegner activity level improved to level 8 in 1 case, level 7 in 12 cases, level 6 in 18
170 cases and level 5 in 9 cases.
171 At six-months follow-up 29 cases in MDB group and 21 cases in SB group could return to preinjury Tegner
172 activity level. At one-year 37 (92.5%) cases in MDB group achieved their pre-injury Tegner activity level as
173 compared to 26 (60%) in SB group.
At one-year follow-up graft was found intact in all cases of both groups on MRI (Fig. 5). Even after two years
175 there was no instability till final follow-up in both groups.
Discussion
178 Stability was achieved in all cases in both groups after ACLR. Objective measurements of anterior tibial
179 translation showed significant improvement in both groups at follow-up in comparison to preoperative
180 status. Though none of the case in either group had complaint of subjective instability in postoperative
181 period, the objective improvement of anterior tibial translation (ATT) in MDB group was better than SB
182 group and was statistically significant (p < 001). Objective measurement of ATT is strength in this study as
183 the results of previously reported studies were based only on subjective scoring in clinical setting and ATT
184 could only be measured at time zero in lab setting. Wider foot print of ACL insertion provides better
stability, which is a case with MDB technique as it provides wide footprint on tibia. The advantage is
186 depicted by significantly better ATT in MDB group as compared to SB group. The Pivot shift test was
negative in both groups but it is difficult to appreciate minor difference in pivot shift in a wake patient in
188 clinic. It has been established by cadaveric studies that the native ACL has a bigger tibial footprint than
femoral foot print.14,15 In cadaveric study Iriuchishima et al.14 189 reported that tibial foot print of ACL 133.8 ±
31.3) mm is nearly twice the size of femoral foot print (69.8 ± 25.0) mm.
There was statistically significant improvement in postoperative IKDC and Tegner activity scores in both
192 groups as compared to preoperative status. But improvement of IKDC score in MDB group was
193 significantly better than SB group (p value<0.001). Return to preinjury status, it was better in MDB group in
194 comparison to SB group as depicted by better Tegner scale.
195 Though authors of previous studies have reported satisfactory outcome with this technique, there was no
control group for comparison to modified DB ACLR in clinical setting.5-9
Papachristou et al.5 197 used suspensory fixation on both sides but we used interference fixation on femoral side
198 and implant less suspensory fixation on tibial side in form of graft loop over bone bridge on tibia.
Sacramento et al.16 199 have also reported implant less fixation over tibial bone bridge in DB ACLR. They have
tied the free suture ends of graft in anteromedial and posterolateral tunnel over bone bridge in 20o 200 knee
201 flexion.
Tibial fixation site is a potential weak link in ACLR with the risk of graft slippage in early postoperative
203 period. Though there was no case of tibial fixation side failure in either group, we feel that looped graft over
204 tibial bone bridge (between anteromedial and posterolateral tunnel) at external aperture in MDB group is
205 more secure. The looped construct of graft over bone bridge in tibia also provides advantage of implantless
206 fixation as well as eliminates chances of graft pulling-out from tibia in rehabilitation period. If the harvested
207 graft is small that can happen with Gracillis, it can be lengthened using an extension loop of fibre wire. This
208 loop remains outside the tunnel over the bone bridge of the tibia. But in this study graft length was not a
209 problem and extension loop was not required in any case in MDB group.
13 without any case of failure on femoral side in either group. One of the strength of MDB technique is that all
214 the tunnels are occupied with graft giving more graft bone contact surface area for better healing.
Most studies recommend fixation of posterolateral bundle in 10o
-20o
215 of flexion and that of anteromedial
bundle in 70 o-90o flexion6
including Papachristou et al5
. Park et al.7
216 fixed posterolateral bundle at full
extension and anteromedial bundle at 45o 217 flexion. Fixation of both bundles was performed in knee flexion of
20o
by Naser9
, 30o by Yasuda et al.17 and 20 o by Sacramento et al.16. We fixed both bundles in 10o
218 of knee
219 flexion. It was based on the fact that anteromedial bundle is more isometric than posterolateral bundle
making it taut in whole flexion range but posterolateral bundle is taut in only first 30o
220 knee flexion. One of
221 the advantages of reported technique over other implantless tibial fixation techniques is no risk of loss of
222 tension in graft while fixing it as interference fixation is done at the same time when assistant holds the graft
223 in tension.
224 One of the advantages of MDB ACLR over SB ACLR is there is no tibial fixation required that minimizes
225 the hardware and cost of the procedure.
226 There was no complication in MDB and SB groups. The only drawback of MDB over SB group was
227 increased tourniquet time.
Weakness of the study is non-randomized case recruitment.
229 In conclusion, the MDB ACLR has shown significantly better short-term clinical outcome as compared to
230 the SB ACLR. The graft construct is close to native ACL. It is a simple and reproducible technique that does
231 not require fixation on tibial side and thus minimizes the cost.
Funding
234 Nil.
235 Ethical Statement
236 This prospective study was conducted after institutional approval.
237 Declaration of Competing Interest
238 On behalf of all authors, the corresponding author states that there is no conflict of interest.